Educating and Empowering You to Heal, Thrive, and Live a Happy, Healthy Lifestyle
Causes for Thyroid Problems and Thyroid Disorders
 Thyroid problems are increasingly common nowadays. Many people have no idea that they have an underlying thyroid imbalance, thyroid dysfunction or thyroid autoimmunity (Hashimoto’s thyroiditis or Grave’s disease). In addition, thyroid problems are frequently under-diagnosed and misdiagnosed.
Thyroid problems are increasingly common nowadays. Many people have no idea that they have an underlying thyroid imbalance, thyroid dysfunction or thyroid autoimmunity (Hashimoto’s thyroiditis or Grave’s disease). In addition, thyroid problems are frequently under-diagnosed and misdiagnosed.
Thyroid hormone is the master metabolism hormone. The thyroid gland is intrinsically connected with metabolism, brain functioning, and energy levels. If your thyroid is out of balance, your metabolism, brain function, energy and entire body chemistry will also be out of balance.
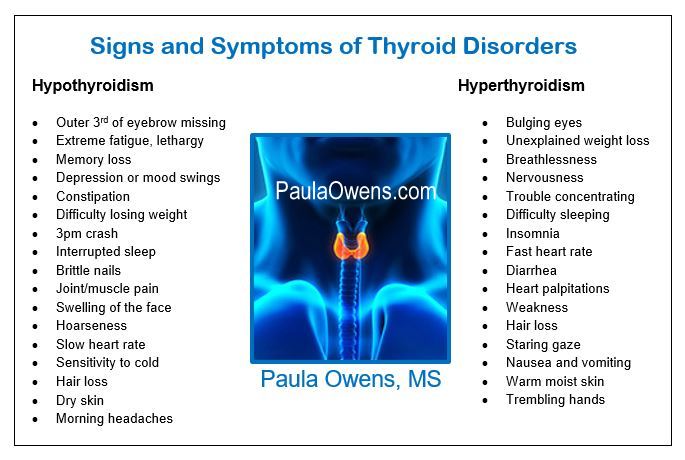
Those with hypothyroid often tend to have high cholesterol, a congested liver, sluggish bile, multiple nutrient deficiencies, digestive problems, adrenal insufficiency, heavy metal toxicity, food sensitivities, hidden infections, and undiagnosed Hashimoto’s.
Oftentimes, those with thyroid problems are treated with Synthroid, cholesterol-lowering statin drugs, anti-anxiety medications and antidepressants instead of accurately assessing, balancing and restoring adrenal, gut and thyroid function.
Common scenario: you’ve been told your thyroid is perfectly ‘normal’ even though only TSH was tested, and you’re experiencing several thyroid symptoms.
Causes for Thyroid Problems and Thyroid Disorders
Hashimoto’s thyroiditis, an autoimmune disease is the number one cause of thyroid problems and the most common cause of hypothyroidism. Unfortunately, Hashimoto’s is frequently undiagnosed and is often missed by a standard TSH test.
Your diet. Processed foods that are low in nutrients and high in chemicals, calorie restriction, low-fat diets, skipping meals, protein deficiency, lack of food diversity, and complete avoidance of healthy carbs increase the risk of thyroid problems. (download the healthy food guide)
- When too little protein or the wrong kind of protein is eaten, there is a stress reaction with thyroid suppression.
- A gluten-free, soy-free, dairy-free and grain-free diet is a life changing intervention for those suffering with any type of thyroid disease.
- Eggs (although a very nutrient-dense food) can be problematic for some, creating an inflammatory, immune reaction.
- Nightshades and high-lectin containing foods can also be problematic. Beans, grains, legumes and members of the nightshade family like eggplants, potatoes and peppers.
- Food sensitivity testing (IgG), a valuable test to detect and assess an individual’s personal food sensitivities (an inflammatory insult to the thyroid) can be a game changer.
GI dysfunction, intestinal permeability (leaky gut) and poor digestion. A large portion of thyroid conversion happens in the gut. Absorption problems due to low stomach acid (hypochlorhydria) and low digestive enzymes, inflammatory bowel disease, Celiac disease, and an inflamed, leaky gut can cause several nutrient deficiencies that cause thyroid problems and the ability to make thyroid hormones.
Sluggish bile (gallbladder dysfunction). There is a direct relationship between hypothyroidism, gallbladder dysfunction and gallstone disease. Hypothyroidism is seven times more likely in those with sluggish, impaired bile. [Tampere University Hospital in Finland] A 2016 study concluded that “thyroid dysfunction is more common among patients with gallstones and it may be a risk factor for biliary stone formation.”
Congested liver. Anything that impairs liver function directly affects hormonal balance, including healthy thyroid function. A healthy liver is crucial for the conversion of T4 into the active form T3 conversion. It’s estimated that 80% of thyroid conversion happens in your liver and 20% in your gut.
Poor liver detoxification hinders the conversion of T4 to T3, and also prevents the elimination of excess estrogen. As a consequence, excess estrogen leads to an overabundance of the thyroid-binding proteins that transport thyroid hormones through the bloodstream. Too many thyroid-binding thyroid hormones prevent thyroid hormones from getting into the cells resulting in hypothyroid symptoms.
Hidden infections must be ruled out with thyroid problems. Viral infections such as Epstein-Barr (EBV), old root canals, dental infections, sinus infections, H. pylori, Yersinia, parasites, Candida overgrowth, yeast overgrowth, fungi, Lyme, mold, SIBO, bacterial infections such as Klebsiella, Citrobactor and many others
Environmental triggers, endocrine disruptors, obesogens and metabolism disrupting chemicals found in the air, the water, food, skincare products, household cleaning products, personal care products, cosmetics, detergents, fabric softeners and dryer sheets, water and food containers, pesticides, and more are causing an increase in thyroid dysfunction, mitochondrial dysfunction, cardiometabolic problems, neurological dysregulation and autoimmunity—and, complex illness is a consequence.
We’re living in a sea of toxic chemicals and exposed to more chemicals in a 30-day period than our grandparents were exposed to in their entire lifetime.
Endocrine disrupting chemicals have been renamed metabolism disrupting chemicals because they not only disrupt hormones, they also disrupt nuclear receptor sites in the nucleus of the cell.
Thyroid disrupting chemicals from Teflon cookware, flame retardants, plastics, PCBs, pesticides, phthalates, BPA, GMOs, glyphosate, formaldehyde, triclosan, petrochemicals, EBDCs (a group of carcinogenic, anti-thyroid fungicides), xenoestrogens and other endocrine disrupting chemicals. Research has shown that some pesticides promote the formation of thyroid nodules.
There’s clinical research that shows that there is a direct correlation between PCBs, phthalates, BPA and plastics and thyroid problems. The higher the levels of BPA, plastics and phthalates are in the urine, the lower the levels are of total T4 and total T3, and the higher the level of TSH.
Unfiltered water. Filtered water is a necessity as the presence of harmful chemicals, toxic metals and fluoride or chlorine in water block the iodine receptors in the thyroid gland and aggravate thyroid problems.
Halogens: chlorine, fluoride and bromide/bromine
- Fluoride found in toothpaste, tap water, non-stick compounds and various antibiotics and medications. Fluoride competes with iodine which is necessary to make T4.
- Chlorine in swimming pools, hot tubs, bleach, tap water, and pesticides
- Bromide found in bread, flame retardants, hot tubs, Mountain Dew soda pop
Toxic heavy metals such as mercury, cadmium, lead, arsenic, aluminum and other heavy metals that cause thyroid problems.
Environments that have elevated levels of toxic heavy metals, pesticides, BPA, PCBs have been associated with an increase in anti-TPO antibodies as PCBs mimic thyroid hormones, and interrupt biochemical competency (Duntas, 2008). Increased oxidative stress and a high toxic load are common with an enlarged thyroid.
Disrupted circadian rhythms. Your thyroid health is influenced by circadian rhythms. Circadian dysfunction caused by shift work, travel across time zones or irregular sleep–wake cycles is a lifestyle risk factor for thyroid dysfunction and an increased risk of thyroid cancer. Nature Reviews Endocrinology 2019.
Sunlight deficiency. Getting the proper amount of daily sunlight is vital for improving thyroid function, vitamin D, immunity, sleep quality, and regulating your circadian rhythm.
Radiation and EMF exposure. The thyroid gland is particularly sensitive and susceptible to the effects of electropollution and electromagnetic radiation (EMR) including x-rays and other forms of radiation. Increased exposure to cell phone radiation, wireless devices, EMFs, WiFi, 5G and electrosmog affect TSH and thyroid metabolism.
Breast implants. Silicone, plastics, saline, toxic metals and other foreign toxic fillers can leach out over time causing thyroid problems and other illnesses.
Nutrient deficiencies. The most common nutrient deficiencies that I find in those with thyroid dysfunction include omega-3s and other fatty acids, selenium, zinc, iodine, magnesium, tyrosine, vitamin D, vitamin A, and various B vitamins.
Stress, HPA axis dysfunction and adrenal dysfunction. Optimizing adrenal function is a crucial component in treating thyroid dysfunction and autoimmunity.
Stressful lifestyle, sympathetic overdrive, unresolved soul wounds, prior trauma (emotional, mental, physical), compounding episodes of stressful events, poor vagal tone, stress-induced PNEI (psycho-neuro-endocrine-immunological) imbalances impact healthy thyroid function, adrenal function, and trigger thyroid problems and autoimmune progression and flare-ups.
In patients in whom hypothyroidism and severe hypoadrenalism coexist, administration of thyroid hormone prior to correcting adrenal insufficiency can trigger an “adrenal crisis.”
Mental and emotional stress, chemical stress, thermal stress, environmental stress and mechanical stress have a powerful effect on thyroid and other hormones.
Medications linked to thyroid problems
- Excessive thyroid hormone (side effects may include anxiety, insomnia, heart palpitations, nervousness, rapid pulse, pain or tightness in the chest)
- Incorrect thyroid prescription. If you’re taking prescription thyroid, make sure that it is dosed specific to your body chemistry. Like diet, there is no one-size-fits-all thyroid medication for everyone. Not all thyroid meds work the same for every person.
- Accutane
- Amiodarone (used to treat ventricular tachycardia, ventricular fibrillation, tachycardia, as well as atrial fibrillation and paroxysmal supraventricular tachycardia)
- Antacids, PPIs (proton pump inhibitors), acid-blocking drugs
- Antibiotics
- Anticoagulants (blood thinners)
- Antidepressants, bipolar medications and lithium
- Anti-seizure medications
- Beta blockers for hypertension
- Botox
- Cholesterol-lowering statin drugs
- Cholestyramine
- Estrogen hormones: birth control pills, Mirena IUD, hormone replacement therapy (HRT and BHRT). Increased estrogen has been associated to thyroid cancer.
- Excessive iodine intake
- Fluoride-containing drugs
- Interferon
- Narcotics and pain medications, Tylenol, NSAIDs
- Vaccine ingredients
Hormonal imbalances. It’s important to factor in other hormonal imbalances when evaluating thyroid dysfunction. Insulin resistance, blood sugar imbalances, high or low cortisol, and estrogen dominance are linked to hypothyroidism.
Elevated estrogen directly affects thyroid function by hindering the liver’s conversion of T4 to active T3, and by increasing levels of thyroid-binding proteins, which limits the amount of free thyroid hormone to enter the cells.
Hormonal fluctuations that occur during perimenopause, menopause, andropause, recent pregnancies, postpartum thyroiditis, after childbirth and during lactation impact thyroid function.
Thyroid testing. In addition to TSH, it’s important that free T4, free T3, reverse T3 and thyroid antibodies are included with your thyroid panel. If your doctor refuses to test your antibodies, you can order these yourself through my online lab portal, which is very affordable.
For my own thyroid imbalance, nourishing my adrenals, supporting my body chemistry with targeted nutrients, and addressing the heavy metal toxicity were key players. To heal your thyroid, working with an experienced practitioner will help you identify your personal nutrient deficiencies, the root causes, underlying imbalances, inflammatory insults and environmental triggers, and design a lifestyle plan to balance your body chemistry, restore healthy thyroid function, and heal your whole body. Schedule a free 15-minute consultation!
Related Posts
- Video: Have Any of These Symptoms?
- How to Support Hypothyroid
- Root Causes for Hashimoto’s and other Autoimmune Diseases
- Testimonial: How I Reversed Hashimoto’s
- Testimonial: I no longer need to take blood pressure drugs or thyroid medication

